February 11, 2020, by NCI Staff

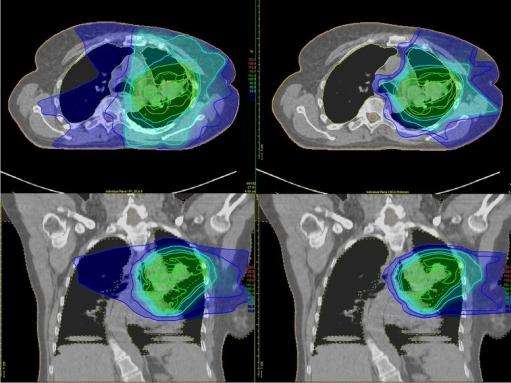
Traditional radiation therapy (top and bottom left) delivers radiation to the tumor and to healthy tissues around the tumor. With proton therapy (top and bottom right), the majority of the radiation is delivered to the tumor.
Credit: Trials. November 2016. doi: 10.1186/s13063-016-1679-4. CC BY 4.0.
A type of radiation treatment called proton beam radiation therapy may be safer and just as effective as traditional radiation therapy for adults with advanced cancer. That finding comes from a study that used existing patient data to compare the two types of radiation.
Traditional radiation delivers x-rays, or beams of photons, to the tumor and beyond it. This can damage nearby healthy tissues and can cause significant side effects.
By contrast, proton therapy delivers a beam of proton particles that stops at the tumor, so it’s less likely to damage nearby healthy tissues. Some experts believe that proton therapy is safer than traditional radiation, but there is limited research comparing the two treatments.
Plus, proton therapy is more expensive than traditional radiation, and not all insurance companies cover the cost of the treatment, given the limited evidence of its benefits. Nevertheless, 31 hospitals across the country have spent millions of dollars building proton therapy centers, and many advertise the potential, but unproven, advantages of the treatment.
In the new study, patients treated with proton therapy were much less likely to experience severe side effects than patients treated with traditional radiation therapy. There was no difference in how long the patients lived, however. The results were published December 26 in JAMA Oncology.
“These results support the whole rationale for proton therapy,” said the study’s lead investigator, Brian Baumann, M.D., of the Washington University School of Medicine in St. Louis and the University of Pennsylvania.
But key aspects of the study limit how broadly the findings can be interpreted, said Jeffrey Buchsbaum, M.D., Ph.D., of NCI’s Radiation Research Program, who was not involved in the study.
Because of those limitations, “the evidence needed to truly justify the expenses of proton therapy … will need to come from phase 3 randomized clinical trials,” wrote Henry Park, M.D., and James Yu, M.D., of Yale School of Medicine, in an accompanying editorial.
Several NCI-funded randomized clinical trials comparing proton and traditional radiation therapy are currently ongoing. (See the box below.)
Safety and Efficacy of Proton Therapy
Many people with locally advanced cancers are treated with a combination of chemotherapy and either traditional or proton radiation. For patients getting chemotherapy and radiation at the same time, finding ways to limit side effects without making the treatment less effective is a high priority, Dr. Baumann said.
He and his colleagues analyzed data from nearly 1,500 adults with 11 different types of cancer. All participants had received simultaneous chemotherapy plus radiation at the University of Pennsylvania Health System between 2011 and 2016 and had been followed to track side effects and cancer outcomes, including survival. Almost 400 had received proton therapy and the rest received traditional radiation.
Those who received proton therapy experienced far fewer serious side effects than those who received traditional radiation, the researchers found. Within 90 days of starting treatment, 45 patients (12%) in the proton therapy group and 301 patients (28%) in the traditional radiation group experienced a severe side effect—that is, an effect severe enough to warrant hospitalization.
In addition, proton therapy didn’t affect people’s abilities to perform routine activities like housework as much as traditional radiation. Over the course of treatment, performance status scores were half as likely to decline for patients treated with proton therapy as for those who received traditional radiation.
And proton therapy appeared to work as well as traditional radiation therapy to treat cancer and preserve life. After 3 years, 46% of patients in the proton therapy group and 49% of those in the traditional radiation therapy group were cancer free. Fifty-six percent of people who received proton therapy and 58% of those who received traditional radiation were still alive after 3 years.
Limitations of the Study’s Design
The study leaders and other experts noted several limitations to the study’s design.
For instance, this observational study can’t establish a cause-and-effect relationship between proton therapy and fewer side effects. In addition, all of the study participants were treated at a single institution, which can make it difficult to generalize the findings to a larger population.
“Those are very significant limitations that shouldn’t be understated,” Dr. Buchsbaum emphasized.
Although single-institution studies have inherent limitations, Dr. Baumann noted, all patients in this study received high-quality treatment at a large academic medical center, regardless of whether it was proton or traditional radiation therapy, “which suggests that the benefit of proton therapy that we saw is meaningful.”
Also, because patients were not randomly assigned to treatment groups, there were differences between patients who got proton and traditional radiation, and that may have skewed the results.
For instance, patients who received proton therapy were, on average, older (likely because Medicare typically covers the cost of proton therapy) and had more health issues.
The proton therapy group may also have included more patients from “privileged backgrounds,” Drs. Park and Yu noted. Socioeconomic status and social support can affect treatment outcomes, they wrote.
In addition, fewer people with head and neck cancer—who are more likely to suffer from radiation-associated side effects—were included in the proton therapy group, the editorialists added.
In their analysis, the investigators used complex statistical techniques to try to account for these differences as much as possible.
Ideas for Future Studies of Proton Therapy
Despite the study’s limitations, these “intriguing findings raise questions that should inform future prospective phase 3 trials,” Dr. Buchsbaum said, although there are barriers to large studies of proton therapy.
For instance, it “is particularly encouraging” that proton therapy appeared to be safer in a group of older and sicker patients who typically experience more side effects, Dr. Baumann noted.
Dr. Buchsbaum agreed that proton therapy may be especially helpful for older and sicker patients, but he noted that ongoing phase 3 trials were not designed to analyze this group of patients.
And because proton therapy may cause fewer side effects, future trials could also explore whether combining proton therapy with chemotherapy might be more tolerable for patients, the authors wrote.
For example, both chemotherapy and traditional radiation for lung cancer can irritate the esophagus, making it painful and difficult for patients to eat. But proton therapy might limit damage to the esophagus, making it easier for a patient to tolerate the combination, Dr. Baumann explained.
Future studies could also explore whether combining proton therapy with higher doses of chemotherapy might increase cures without causing more side effects, he added.
The study findings also raise “the tantalizing possibility that the higher up-front cost of proton therapy may be offset by cost savings from reduced hospitalizations and enhanced productivity from patients and caregivers,” the study researchers wrote.
Dr. Buchsbaum agreed, saying that it would be worthwhile to explore this possibility. “Just asking the question: ‘Is [proton therapy] more effective?’ might not be giving it a fair opportunity to demonstrate its benefit to society,” he said.
Dr. Baumann and his colleagues are currently studying the cost effectiveness of proton therapy, considering aspects like the costs of treating side effects and the value of preserved quality of life.
Prostate cancer is the second most common cancer in American men, behind only skin cancer. As of 2022, about one out of every eight men will be diagnosed with prostate cancer at some point during his lifetime. However, it’s rare for those who are younger than 40 to develop prostate cancer. Nearly six out of 10 prostate cancer patients are over the age of 65. In this article, we’ll explain why proton therapy is an ideal treatment option for many prostate cancer patients.

The prostate surrounds the urethra and is located beneath the bladder. The gland secretes prostate fluid as one of the components for seminal fluid. Cancer begins to develop in the prostate when the cells of the gland begin to grow uncontrollably and form a malignant tumor. If left untreated, prostate cancer can spread to other parts of the body such as the bladder, rectum, bones, and lymph nodes, where it can become life-threatening.
Fortunately, modern medicine has made the survival rates of prostate cancer fairly high. The American Cancer Society reported in 2022 that more than 3.1 million Americans previously diagnosed with prostate cancer are still alive and well today.
Common Types of Prostate Cancer
The majority of prostate cancer diagnoses involve adenocarcinomas, or cancers which develop immediately within the gland cells. It is possible to develop other types of prostate cancer, including:
- Ductal adenocarcinoma – begins in the ducts of the prostate gland
- Transitional cell cancer – begins in the bladder and spreads to the urethra, prostate, and nearby tissues
- Squamous cell cancer – begins in the flat cells of the prostate gland
- Small cell prostate cancer – a type of neuroendocrine cancer made up of round, small cells
Additional types of prostate cancer such as sarcomas and carcinoid are considered extremely rare. Those who are diagnosed with prostate cancer are likely to have adenocarcinomas.

Risk Factors and Prevention
Risk factors such as age, ethnicity, and family history have been known to influence the chances of a person developing prostate cancer. However, it should be noted that risk factors don’t have a direct impact on the development of cancer.
Men over the age of 50 are more likely to develop prostate cancer. In fact, 80% of people who are diagnosed with prostate cancer are over the age of 65.
According to the CDC, African American men are more likely to be at risk for prostate cancer and are more likely to develop aggressive tumors. On the other hand, Caucasian men are just under the average rate of prostate cancer diagnoses. Likewise, Hispanic men also have a lower risk. People of Asian and Pacific Islander descent have the lowest risk of developing prostate cancer.
A family history of prostate cancer can also have an impact on your chances of developing cancer. Only 5% of prostate cancer cases are inherited, but up to 20% of cases are familial, meaning common lifestyle factors and shared genes may have had an influence on the development of cancer.
While risk factors don’t have a direct impact on the development of prostate cancer, they can motivate you to monitor your lifestyle more closely. To lower your risk of developing prostate cancer, it’s recommended to eat a low-fat diet and exercise regularly. However, it’s best to monitor your health by receiving routine checkups and prostate screenings from your doctor.
Proton Therapy Treatment for Prostate Cancer Patients
Proton therapy is a form of radiation treatment for cancer patients. Also called proton beam therapy, proton therapy involves focusing proton particles into a beam, which is then delivered to the cancer cells in a non-surgical procedure. The positively charged particles can be controlled to stop at the tumor site, enabling the cancerous tissues to be destroyed with high levels of radiation without causing damage to nearby healthy tissue and vital organs. Proton therapy is considered more precise than other types of radiation therapy. It is also non-surgical, non-invasive, and has minimal side effects. Proton therapy treatment requires little to no recovery time, and the radiation has very little impact on a patient’s energy level compared to other cancer treatment options.
Proton therapy exhibits higher success rates in prostate cancer patients.
According to a study published by the University of Florida, prostate cancer patients who received proton therapy treatment were found to be free of cancer progression for five years after their treatment. Patients with low to medium risk prostate cancer experienced a success rate of 99%, while those with high risk prostate cancer experienced a success rate of 76%.

Proton Therapy vs. Traditional Radiation Therapy
So, what makes proton therapy so much more successful than other prostate cancer treatments? The answer lies in the protons themselves.
Unlike proton therapy, traditional radiation treatment uses photons, which deliver low levels of radiation to the cancer tissues. These lower levels of radiation, in addition to the lower mass of the beam in comparison to a proton treatment, mean the radiation will cause damage to both the cancerous tissue and the surrounding healthy tissue.
On the other hand, proton therapy uses positively charged subatomic particles called protons, which are located in the nucleus of an atom. Because the mass of the proton beam is higher than the photon beam, a clinician can control the proton radiation in the patient’s body. The electrons in the patient’s body slow down the protons delivered from the beam. This results in an energy release that can destroy cancerous tissue, but avoid unnecessary radiation to surrounding areas. Unlike traditional radiation therapy, the clinician can use the proton beam to target the cancer cells in the body specifically, allowing for a more successful and far less damaging procedure.
Proton Therapy Is Proven to Enhance Quality of Life
According to a national survey, patients who received proton therapy to treat their prostate cancer reported experiencing a better quality of life with regard to urinary and bowel function during and after proton therapy, compared to those who received traditional radiation. Additionally, more than 70% of prostate cancer patients who received proton therapy noted the treatment had no impact on their quality of life overall.

Two studies conducted by the University of Texas confirm that patients who receive proton therapy treatments for prostate cancer show an improved quality of life compared to those who choose other treatment options.
“In general, patients are interested in learning how they will do compared to those treated with other modalities, but, more importantly, they want to know how they are going to do, relative to their own normal state of health,” said Andrew K. Lee, M.D., who led both studies. “With such a large data set, this study offers us a guide to have that discussion with patients considering proton therapy.”
97% of survey respondents who chose proton therapy treatment for their prostate cancer said they would recommend it to other patients, as well.

Proton Therapy Success Stories
It’s one thing to hear about the success rate of proton therapy treatment for prostate cancer. It’s another thing to hear the success stories straight from the mouths of survivors.
 Wally K.
Wally K.
Wally, an Army pilot, biker, and all around adventurer, was diagnosed with prostate cancer only six weeks after being prescribed testosterone for his anemia.
“There are unending volumes in thousands of books that attempt to describe the kaleidoscope of feelings and emotions that follow a diagnosis of metastatic cancer,” said Wally in his journal entitled the Proton Chronicles. “I’m sure that like many, I attempted to rationalize or even justify the situation, but when faced with real mortality, your life and that of your family is forever altered.”
After considering surgery and consulting multiple online forums, Wally finally decided on proton therapy to treat his cancer. Over the course of 20 hypofractionated treatments, Knight continued to bike on his favorite trails and play hockey in the local ice rink.
“It’s really kind of difficult to get your head around the whole situation,” said Knight about his proton treatment. “This is happening at the cellular level and it’s absolutely painless.”
 Earl M.
Earl M.
Earl, a mission pilot and pastor, also received proton therapy after being diagnosed with prostate cancer. Having lived in Alaska for nearly two decades with his wife, Lynn, he chose to seek medical care in other states after receiving his diagnosis.
After consulting multiple cancer centers and discussing his options with a doctor who incorrectly referred to proton therapy as experimental, Earl chose to receive treatment at Provision CARES Proton Therapy.
“It was first-class,” said Earl about Provision. “They helped me, and they also had an impact on my wife and son, and the families we serve up in Alaska. They have an impact far greater than you can imagine.”