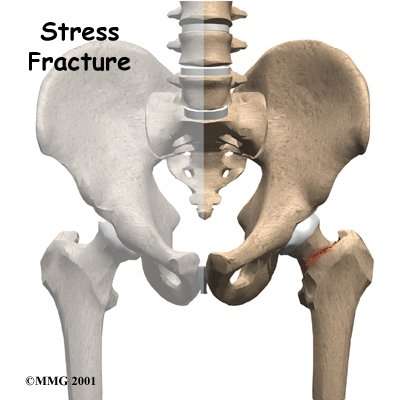
The femur is the large bone in the thigh. The ball-shaped head of the femur fits into a socket in the pelvis, called the acetabulum. When a stress fracture occurs in the hip, it usually involves the femoral neck, the short section of bone that connects the head of the femur to the main shaft of the bone. The femoral neck is a thinner part of the femur. Stress fractures are hairline cracks in the bone that can grow larger over time if not treated properly.
Hip
The femoral neck has to withstand extreme force even during normal activities, such as standing still. The normal contraction of muscles during walking makes this stress even higher. Running triples the stress on the femoral neck.
Surgeons put fatigue fractures of the femoral neck into three categories. Compression fractures occur on the underside of the femoral neck. Tension fractures occur on the upper side of the bone and can cause more problems than fractures on the underside of the femoral neck. In displaced fractures, the bone cracks all the way through, and the two bones no longer line up correctly.
Three Categories
A displaced stress fracture is a very serious problem in a young adult because it may lead to damage to the blood vessels going into the upper end of the hip bone. This can cause a very serious complication known as avascular necrosis (AVN) of the hip.
Related Document: Therafit Physical Therapy’s Guide to Avascular Necrosis of the Hip
Patients with fatigue stress fractures of the hip are also likely to have muscle and tendon injuries and swelling of the synovial lining (the lubricated lining) of the hip joint.
Stress fractures can also happen in the shaft of the femur bone, the greater trochanter, and the pelvis bone. The greater trochanter is a large bump below the neck of the femur. The buttock muscles that move the hip connect to this part of the femur.
Greater Trochanter
Related Document: Therafit Physical Therapy’s Guide to Hip Anatomy
For access to all of our training, gear, and race coverage, plus exclusive training plans, FinisherPix photos, event discounts, and GPS apps, sign up for Outside+.
How to treat and prevent the dreaded hip stress fracture.
Pain in the hip joint (sometimes perceived as groin pain) that worsens at the foot strike when running or hopping on just that leg can signal a hip stress fracture. It can also hurt when lying down. With continued activity, the pain usually gets worse over time.
Hip injuries are common in all athletes, but this type of injury is especially common in runners and triathletes. A femoral neck stress fracture—a crack near the ball at the top of the femur—is the most serious. Stress fractures are almost always caused by overuse, usually by runners who try to “load” miles too fast in preparation for a big race. The bone simply cannot take the pounding.
If you have this type of pain, here are two questions to ask yourself: Have I upped my training workload too fast, too soon? And, how is my bone density? These aren’t the only two factors involved, but they are the most common.
Low bone density (osteopenia) or very low bone density (osteoporosis) have several possible causes: genetics, as it tends to run in families; inadequate dietary calcium intake (1,300 milligrams a day is the recommended minimum); and for women, a history of menstrual disorders (e.g., not getting a period for more than six months can cause a low level of circulating estrogen).
The good news is that these variables can be altered or compensated for to help alleviate the problem.
RELATED: Stress Fracture Treatment And Prevention
Fix It
Employ dynamic rest. Stop any activity that impacts the hip joint. Use intense upper-body and core workouts to maintain fitness.
Supplement. Eat more calcium- and vitamin D-rich foods or take supplements.
Slowly strengthen. Your lower body will need some work once you’re ready to resume activity. When you are pain free, gradually add lower-body strengthening exercises back into your workouts. Multi-directional lunges and squats will help, but avoid high-impact activity until your doctor gives you the all clear.
RELATED: Why Should Take Care Of Your Kinetic Train
Prevent It
Up your calcium and vitamin D intake. Easy food sources are milk and yogurt; or take supplements. This is especially important if you have a family history of osteoporosis.
Follow the 10 percent rule. Never up your weekly running mileage by more than 10 percent.
Train your hips and core. The stronger the muscles in your core, glutes, hips and legs are, the more support your hip joints will have against repetitive impact. Make sure planks, multi-directional lunges, squats, squat jumps and skater plyos are a regular parts of your workouts.
New York City sports medicine specialist Jordan D. Metzl, M.D. is a 33-time marathon finisher and 13-time Ironman. His book, The Athlete’s Book of Home Remedies, has more than 1,000 tips to fix all types of injuries and medical conditions.
Introduction
Stress fractures of the hip are more common in athletes, especially distance runners. There are two types of stress fractures. Insufficiency fractures are breaks in abnormal bone under normal force. Fatigue fractures are breaks in normal bone that have been put under extreme force. Fatigue fractures are usually caused by new, strenuous, very repetitive activities, such as marching or distance running. Most stress fractures of the hip are fatigue fractures. The stress fractures referred to in this article are fatigue fractures.

Anatomy
The femur is the large bone in the thigh. The ball-shaped head of the femur fits into a socket in the pelvis, called the acetabulum. When a stress fracture occurs in the hip, it usually involves the femoral neck, the short section of bone connecting the head of the femur to the main shaft of the bone. The femoral neck is a thinner part of the femur. Stress fractures are hairline cracks in the bone, which can grow larger over time if not properly treated.

The femoral neck has to withstand extreme force even during normal activities, such as standing still. The normal contraction of muscles during walking makes this stress even higher. Running triples the stress on the femoral neck.
Doctors put fatigue fractures of the femoral neck into three categories. Compression fractures occur on the underside of the femoral neck. Tension fractures occur on the upper side of the bone and can cause more problems than fractures on the underside of the femoral neck. In displaced fractures, the bone cracks all the way through, and the two bones no longer line up correctly.

A displaced stress fracture is a very serious problem in a young adult because it may lead to damage to the blood vessels going into the upper end of the hipbone. This can cause a very serious complication known as avascular necrosis (AVN) of the hip. Avascular necrosis of the femoral head causes damage to the blood vessels restricting blood flow to the femoral head. This causes the bone in the femoral head to die.
Patients with fatigue stress fractures of the hip are likely to have muscle and tendon injuries and swelling of the lubricated lining (synovial lining) of the hip joint.
Stress fractures can also happen in the shaft of the femur bone, the greater trochanter, and the pelvic bone. The greater trochanter is a large bump below the neck of the femur. The buttock muscles that move the hip connect to this part of the femur.
Causes
Putting extreme stress on the bone over and over again may cause stress fractures of the hip. Bones can usually adapt to repetitive stress, and any change in the function of a bone causes it to change the way it is built. This is how small bumps and ridges form on bones. The tendons pull on these areas, and the bone adapts by building up. This is normal. But, extreme repeated stress may overwhelm the bone’s ability to adapt. This is especially true when someone suddenly begins a new, strenuous, repetitive activity such as running.
Fatigue fractures are related to both the amount of exercise and how fast people increase their exercise program. Research suggests most athletes who develop stress fractures have been training for at least two years, six or more times a week. A stress fracture is more likely to occur after an increase in how far, how often, and how hard a person exercise.
Women are up to ten times more likely to develop fatigue fractures than men. The reasons for this are unclear. Hormonal changes may make women athletes’ bones more likely to fracture. Eating disorders, which are more common in women athletes, may also make bones more likely to fracture.
Age also makes stress fractures of the hip more likely. This is thought to be due to declining levels of physical fitness more than age.
Symptoms
Most patients with stress fractures of the hip feel pain in the front of the groin while standing and moving. Rest usually makes the pain go away. Patients may limp. Strenuous activities, such as running and climbing stairs, may be so painful the patient must stop doing them.

Diagnosis
Your doctor will take a detailed medical history and ask many questions about your activities and exercise. Your doctor will also physically examine the painful hip. One of the doctor’s main goals will be to determine if other problems, such as muscle or tendon injuries, are causing some or all of your pain.
Your doctor will probably suggest taking an X-ray of the affected hip. The X-ray may help rule out other problems, but it probably will not show the stress fracture.
Your doctor may recommend other imaging tests more likely to show a stress fracture. A bone scan may be suggested to look for early signs of a stress fracture. A bone scan involves injecting “tracers” into the blood stream. The tracers then show up on special X-rays of your hip. The tracers build up in areas of extra strain to bone tissue, such as a stress fracture.
The MRI (magnetic resonance imaging) scan is especially useful in telling fatigue fractures from other types of injuries with similar symptoms. The MRI is being used increasingly in cases where doctors suspect a stress fracture.
Treatment
The treatment your doctor recommends will depend on the type of fracture you have.
Conservative Treatment
Doctors most often recommend non-surgical treatment for compression-type fatigue fractures. You must stay off the affected leg, using crutches if necessary, and rest the hip for at least four to six weeks. Pain can be treated with hot and cold treatments and medication. With care, the fractures tend to heal by themselves.
In some patients with a fracture under the femoral neck, MRIs and other imaging tests sometimes show an unstable fracture that needs to be surgically fixed.
Doctors do not all agree on how to treat tension fractures. If the fracture is not at risk for displacing, surgeons may have patients use crutches to keep strain off the hip during standing and walking. X-rays are taken every few weeks to make sure the bone is healing. If the tension fracture is in danger of displacing, most doctors will operate. The displaced fracture may cause AVN with the femoral head actually losing its blood supply and collapsing. This leads very rapidly to degenerative arthritis of the hip joint. Because these effects can be so devastating, most doctors recommend surgery if they feel that the stress fracture is in danger of displacing.
Surgery
The surgical procedure is the same whether the stress fracture is stable or there is only a slight displacement of the bones. If your doctor recommends surgery for a stress fracture of the hip, several large metal screws will be inserted through the femoral neck to hold the fractured bones in place while the fracture heals.
To perform this procedure, a small incision is made on the side of the upper thigh. With the help of a special X-ray machine called a fluoroscope, the surgeon can insert the metal screws into the proper position while watching the X-ray image on a TV screen.

When the ends of the bones show a large displacement, doctors aren’t in total agreement about which surgery is best. Most surgeons agree that younger, active patients benefit if surgery is done to save the femoral head. This method also uses screws to connect the two sections of bone.
To avoid problems with AVN, other surgeons feel that older, less active patients should have part or all of the hip joint replaced. If the socket of the joint is healthy, the surgeon may decide to replace only the ball portion of the joint, a procedure called hemiarthroplasty.
The procedure to replace both the ball and the socket with an artificial joint is called total hip arthroplasty.
Rehabilitation
Treating a stress fracture without surgery requires patients to strictly avoid putting weight down on the foot of the injured leg when they are standing or walking. Some doctors allow their patients to use crutches and touch only their toes down on the injured side. Others prefer their patients rely on crutches to completely avoid putting any weight down.
Your doctor will probably have X-rays taken every few weeks to make sure the bones are lined up and healing. When your doctor sees the bones are healing, you’ll be able to put more weight on your foot as you stand and walk. A physical therapist may direct your rehabilitation to help improve strength and flexibility in the hip and to make sure you are able to safely resume your activities.
Recovery after surgery for hip fracture depends on the type of procedure used. The aim of most surgical procedures for a fractured hip is to help people get moving and walking as quickly as possible. This helps them avoid dangerous complications that can happen from being immobilized, such as pneumonia, blood clots, joint stiffness, and pain.
A physical therapist may work with you in the hospital soon after surgery. Treatments are used to help you begin walking with crutches or a walker, to help you access the bathroom, and gradually improve your hip motion and strength.
During your recovery, you should follow the doctor’s instructions about how much weight you can put down while standing or walking.
After you return home from the hospital, you may have to work with a physical therapist. These visits are to ensure you are safe in and about the home and getting in and out of a car. The therapist will make recommendations about safety, review hip precautions, and make sure a safe amount of weight is placed on your foot when standing or walking.
A few additional visits in outpatient physical therapy may be needed for patients who are still having problems walking or who need to get back to physically heavy work or activities. The therapist’s goal is to help patients maximize hip strength, restore a normal walking pattern, and help them do their activities without risking further injury to their hip.