Atrium Health has the area’s only Level I trauma center – Carolinas Medical Center in Charlotte. That means we provide the highest level of comprehensive care for critically injured patients, and are prepared to respond 24/7 to any type of traumatic injury. This requires that we have in-house acute care surgeons, designated operating rooms, available CT scanners, trauma-accredited nursing staff, surgical critical care, 24/7 blood bank operation and immediately available subspecialists like neurosurgeons and orthopedic trauma surgeons. The center must also participate in trauma prevention programs, have a quality outcomes program, and provide a trauma education and research program.
Our Level II and III trauma centers are also prepared to treat traumatic injuries 24/7, and may transfer the most severe cases to our Level I trauma center. Our MedCenter Air team transports patients who require immediate or critical medical care to Carolinas Medical Center quickly and safely by ground or air.
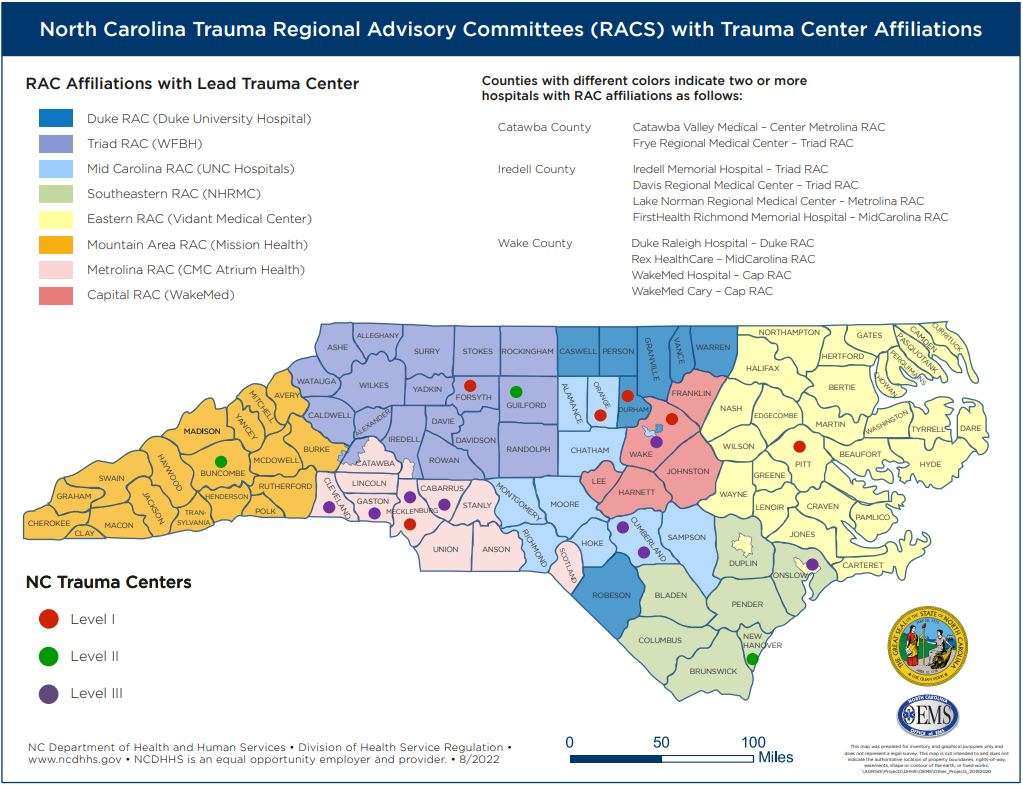
A designated trauma center is a local hospital voluntarily meeting the state’s guidelines for care of the injured patient. Currently North Carolina has 17 designated trauma centers across the state. Each of the state’s centers has the responsibility of providing care, as well as developing and supporting a regional trauma system. Here you can find information related to trauma center designation.
North Carolina Trauma Centers

Click on the map to get to a PDF (106 KB) of the map that will allow you to zoom in on the counties.
Trauma Centers are reviewed, with a site visit, for renewal state designation three years after the initial state designation. Thereafter, a state renewal designation site visit occurs every four years. Should the trauma center wish to obtain or maintain American College of Surgeons (ACS) verification/reverification, they may seek a state renewal designation in conjunction with an ACS site visit every three years to meet the ACS review requirement.
Level I Designation Trauma Centers
Level II Designation Trauma Centers
Level III Designation Trauma Centers
GREENSBORO, NC — There’s only one Level I trauma center in Nevada. Thankfully, it was in Las Vegas. The hospital was swamped with more than 500 people injured and 59 people killed.
In North Carolina we have several Level I trauma centers, one here in the Triad with Wake Forest University Baptist in Winston-Salem. And then there are five more throughout the state; Charlotte, Durham, Chapel Hill, Raleigh and Greenville.
- Carolinas Medical Center—Charlotte
- Duke University Medical Center—Durham
- UNC Hospital—Chapel Hill
- University Health Systems of Eastern Carolina—Greenville
- Wake Forest University Baptist Medical Center—Winston-Salem
Trauma center levels go from I to V.The numbers indicate the resources available in the trauma center and the number of patients admitted yearly. Level I trauma centers are capable of providing total care for every aspect of injury from prevention to rehab.
CHARLOTTE, NC (WBTV) – A horrific car accident. A gunshot wound to the abdomen. When people in the Charlotte region are seriously injured, where do they go? Who cares for the sickest among us?
Enter Atrium Health’s, Level One Trauma center at Carolinas Medical Center in the heart of the city. It’s the only hospital in the region that’s capable to take care of the sickest patients — many of whom come from other hospitals, by ambulance or helicopter.
“Every minute counts so it’s essential for patients to get to the place they need to be very quickly,” said Dr. Susan Evans, the chief of surgical critical care. “In order to be a Level One trauma center, we have a certain set of criteria of things we need to offer.”
It includes doctors, nurses, physician assistants, technicians and surgeons who must be available 24 hours a day, seven days a week – whenever a trauma comes into CMC’s emergency department.
“It’s amazing to see our team just jump into action when we have a trauma code come in. Everybody has a role -and everybody does something important to help save a life,” Dr. Evans said.
Also included in their wide-ranging cases — a new mother of twins whose complications meant a stay in the ICU.
“She was in the ICU because her oxygen level was low and um, her heart rate was high,” said Dr. Evans “But she’s well enough we can take her to see her babies. That’s the part that’s rewarding because it’s kind of the cycle of life. It’s hard to let people die. It’s hard to watch people die. But it’s also exciting to be able to see new life as well.
It’s that new life that keeps this nearly 50-member unit going – especially during the tough calls. As part of a Level 1, they must work together with precision-like teamwork. “When patients come into the trauma bay, someone needs to be putting their heart rate monitor on and their BP monitor on,” she said. “Someone needs to be getting an IV. Somebody needs to be assessing the order of x-rays we might need.”
Usually unconscious because they’re injuries are so grave, Dr. Evans says they relish any opportunity to connect with patients during a trauma call. “If the patient is awake – it’s very helpful if someone can look them in the eye and say, ‘ you’re gonna be ok – we’re going to take care of you’,” she said. “Because that human contact is important for people who are feeling panicky and nervous about how they’re doing and what’s going on.”
But most of the time that human contact is focused on the families especially when they know death is imminent. “It’s incredibly important to me to be able to help the family through that,” Dr. Evans said. “And, I think that there are times when the only care I can give as a doctor is to help a family through the dying process of their loved one.”
While those days never get easier – Dr. Evans says the ones where they reunite with the lives they saved are the most rewarding. “That’s probably the best feeling – seeing somebody who was really sick; maybe we even though they might not survive… so they can come up and say, ‘hi Dr. Evans, thank you very much.’ And that gets my heart more than anything else.”
Other duties for the trauma and surgical critical care team includes emergency surgeries like appendectomies or patients with cancer who have complications that require emergency surgery.
To see an hour by hour look at Dr. Evans’ day as a trauma surgeon, click here.
Copyright 2018 WBTV. All rights reserved.
Overview
Shift Details: 7a – 7p, 24hrs/wk, Weekends
This position is sign on bonus eligible!
The Integrated Enhanced Recovery (ERAS) GI Center of Excellence is composed of a team of physicians, fellows, nurse practitioners and nurses who provide specialized care to patients with diseases of the liver, biliary tract, pancreas and GI tract. As an academic center of excellence in ERAS, opportunities exist to collaborate with institutions nationally and internationally to improve patient outcomes. The nursing department is a specialized unit caring for patients with varying levels of acuity from progressive care, telemetry and medical surgical status. Since these patients will be cared for throughout the entirety of their hospital stay on one-unit, individualized care is integrated into daily work. Progressive care unit experience not required. 11T will be a beacon for clinical advancement and career growth in the field of nursing.
Enhanced Recovery after Surgery (ERAS) is a research-based intensive approach to improving patient outcomes by integrating pathways and guidelines with patient care. Driving compliance, research, quality and publication, this method engages the entire team to align work tailored to improve the patient’s outcome, operational excellence of the organization and experience of the team.
Atrium Health’s Carolinas Medical Center (CMC) is the flagship hospital of Atrium Health, which is distinguished throughout the Southeastern United States for its excellent patient care and medical expertise. CMC serves as the region’s only Level 1 Trauma center, is Magnet-designated, and also an approved transplant center for heart, kidney, pancreas and liver. We also serve as one of North Carolina’s five Academic Medical Center Teaching Hospitals, providing residency training for more than 200 physicians in 15 specialties and serve as a satellite for the medical school at UNC-Chapel Hill.
Job Summary
Provides professional nursing care through skillful assessment, diagnosis, outcomes identification, planning, implementation, and evaluation in accordance with policies and procedures under the supervision of the supervisor and manager. Assists in maintaining a safe work environment and performs all related job responsibilities in a safe manner. Maintains clinical and professional competency as appropriate to the age, culture, developmental stages, and special needs of the patients served.
Provides professional nursing care through skillful assessment, diagnosis, outcomes identification, planning, implementation, and evaluation in accordance with policies and procedures under the supervision of the supervisor and manager. Assists in maintaining a safe work environment and performs all related job responsibilities in a safe manner. Maintains clinical and professional competency as appropriate to the age, culture, developmental stages, and special needs of the patients served.
Essential Functions
- Collects data pertinent to the healthcare consumer’s health or the situation.
- Analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.
- Identifies expected outcomes for a plan individualized to the healthcare consumer or the situation.
- Develops a plan that prescribes strategies to attain expected, measurable outcomes.
- Implements the identified plan, coordinates care delivery, and employs strategies to promote health and a safe environment.
- Evaluates progress toward attainment of goals and outcomes.
- Practices in a manner that is congruent with cultural diversity and inclusion principles.
- Delegates elements of care to appropriate healthcare workers in accordance with any applicable legal or policy parameters or principles.
- Promotes shared governance, or facility decision making activities, developing and nurturing research to positively affect clinical outcomes and promotion.
- Attains knowledge and competence that reflects current nursing practice.
- Integrates evidence and research findings into practice.
- Contributes to quality nursing practice.
- Communicates effectively in all areas of practice.
- Demonstrates leadership in the professional practice setting and the profession.
- Seeks knowledge and competence that reflects current nursing practice and promotes futuristic thinking.
- Evaluates one’s own and other’s nursing practice in relation to professional practice standards and guidelines, relevant statutes, rules and regulations.
- Utilizes appropriate resources to plan and provide nursing services that are safe, effective, and financially responsible.
Physical Requirements
Work requires walking, standing, sitting, lifting, reaching, stooping, bending, pushing, and pulling. Must be able to lift and support the weight of 35 pounds in handling patients, medical equipment, and supplies. Must speak English in good, understandable terms. Intact sense of sight, hearing, smell, and touch. Finger dexterity. Critical thinking and ability to concentrate. Must be able to respond quickly to changes in patient and/or unit conditions. Physical Abilities Testing required. Additional department specific physical requirements may be identified for unique responsibilities within the department by the department leader.
Work requires walking, standing, sitting, lifting, reaching, stooping, bending, pushing, and pulling. Must be able to lift and support the weight of 35 pounds in handling patients, medical equipment, and supplies. Must speak English in good, understandable terms. Intact sense of sight, hearing, smell, and touch. Finger dexterity. Critical thinking and ability to concentrate. Must be able to respond quickly to changes in patient and/or unit conditions. Physical Abilities Testing required. Additional department specific physical requirements may be identified for unique responsibilities within the department by the department leader.
Education, Experience and Certifications
Graduate from an accredited School of Nursing required; BSN preferred. Current Basic Life Support for Healthcare Provider status according to American Heart Association. Current RN license or temporary license as a Registered Nurse Petitioner in the state in which you work and reside or; if declaring a National License Compact (NLC) state as your primary state of residency, meet the licensure requirements in your home state; or for Non-National License Compact states, current RN license or temporary license as a Registered Nurse Petitioner required in the state where the RN works. Additional education, training, certifications, or experience may be required within the department by the department manager.
Graduate from an accredited School of Nursing required; BSN preferred. Current Basic Life Support for Healthcare Provider status according to American Heart Association. Current RN license or temporary license as a Registered Nurse Petitioner in the state in which you work and reside or; if declaring a National License Compact (NLC) state as your primary state of residency, meet the licensure requirements in your home state; or for Non-National License Compact states, current RN license or temporary license as a Registered Nurse Petitioner required in the state where the RN works. Additional education, training, certifications, or experience may be required within the department by the department manager.