Skip slideshow
Girl power: Allyson Berent juggles advancing science with parenting daughters Piper, Quincy, and Kai.
Spectrum/William Mebane

On the go: Quincy, who is nonverbal, uses a tablet to communicate.
Spectrum/William Mebane

Sister act: Kai, 8, presents her picture of progress: a gene therapy, in the form of a heart, entering her sister Quincy’s brain.
Spectrum/William Mebane

Swinging higher: Quincy spent 6 years learning to wave “hello”—like her mother, adversity does not faze her.
Spectrum/William Mebane

Gene genie: James Wilson directs a team at the University of Pennsylvania developing a gene-replacement therapy for Angelman syndrome.
Spectrum/William Mebane

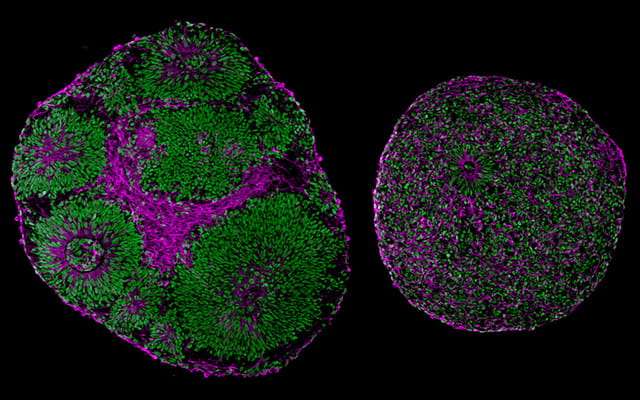
DNA delivery: Researchers test a gene therapy construct for Angelman syndrome.
Spectrum/William Mebane
Originally published on Spectrum
Allyson Berent is a specialty veterinarian in New York City. She treats animals that other doctors cannot help. When no good therapies are available, she invents one. Cats and dogs consumed almost all of her time—until 6 years ago, when her second daughter was born.
As a baby, Quincy appeared healthy and happy, smiling at an early age and giggling frequently. But during her first few months of life, she missed many developmental milestones: At 10 weeks, she was not making eye contact. When her parents waved toys in front of her, she stared blankly. She had trouble feeding. And when she was lying on her stomach, she could not lift her head.
Doctors kept telling Berent and her husband to give it time, but the couple insisted on genetic testing: At 7 months old, their daughter was diagnosed with Angelman syndrome, a neurodevelopmental condition that affects as many as one in 12,000 people.
Most people with Angelman syndrome have severe intellectual disability. They never talk or live an independent life. They experience seizures, gut issues, and sleeping and feeding difficulties. Due to balance and motor problems, they are usually unable or barely able to walk. Many also meet the diagnostic criteria for autism.
Within days of learning her daughter’s diagnosis, Berent set herself a new goal: curing Quincy. With her medical background, she had no trouble parsing the scientific research on Angelman syndrome. She learned that it stems from a missing or mutated copy of a gene called UBE3A, which generates a protein essential for healthy brain activity. People inherit two copies of UBE3A, one from each parent, but the paternal copy is typically silent. In about 70% of people with Angelman, the maternal copy is absent, and they produce none of the protein. Many others with the syndrome have a small mutation in the mother’s copy, rendering it ineffective.
Eager to learn as much as she could, Berent set an alert for “Angelman” in her account with PubMed, the medical journal database. Almost immediately, in December 2014, a paper landed in her inbox that suggested a bold path forward: Researchers had found a way, using snippets of RNA that bind to DNA, to activate the silent copy of UBE3A in a mouse model of Angelman syndrome. And activating the paternal copy of the gene had reversed memory problems in these mice. Could the same thing be done for Quincy? “I went out on a mission to say that I was going to ensure that happened for her,” Berent says.
In March of this year, a child with Angelman syndrome received the first dose of a therapy similar to the one used in the mice. The therapy, dubbed GTX-102, comes from a company called GeneTx Biotherapeutics, founded by Berent and other Angelman parents. Berent also works with a foundation to accelerate other therapies aimed at boosting the missing protein at the heart of Angelman.
GTX-102 is one of a fast-growing number of gene therapies coming to market. Gene therapies replace, repair, activate or silence a gene sequence underlying a condition, rather than addressing its traits. Traditionally, the term “gene therapy” applied only to gene replacement, but as a variety of approaches have shown promise, the phrase has come to refer to all treatments that target DNA or RNA.
Gene therapies are now moving into the autism space, and the Angelman trial is a sign of things to come. “A success in this space will completely change the way that we think about genetic testing in autism,” says Timothy Yu, a neurologist and geneticist at Boston Children’s Hospital in Massachusetts. “It will hold out the idea that if you can name the disease, you can actually do something to improve the quality of life for that child.”
Other companies are developing gene therapies for Angelman that are similar to GTX-102. In late August, Roche launched a clinical trial for its Angelman drug, and a therapy from Ionis Pharmaceuticals and Biogen is nearing human testing. The first gene therapy trial for Rett syndrome, another single-gene condition related to autism, could start as early as next year. And a variety of experimental gene therapies for additional autism-linked conditions, including fragile X syndrome and tuberous sclerosis, are under investigation in animal models. These treatments all target conditions involving just one gene, but some of what scientists learn from developing them pertains to a range of related conditions, including autism that results from more complex causes.
The initial trials of the GeneTx treatment, as with other early-stage tests, are arbiters of safety only. The trial, given the cheeky name KIK-AS, will have just 20 participants, and it will take at least until 2022 before the compound reaches large-scale clinical trials in children, at which point it will be evaluated for its efficacy. Even if a drug passes preliminary testing, it still might not work, or it may work only if started at birth or in the womb.
In other words, it might be too late for Quincy. Berent is clear-eyed about the challenges, but optimistic. “I think this could be ground-breaking,” she says.

Joint effort: Quincy, 6, has applied to participate in a trial of a gene therapy her mother, Allyson Berent, helped develop.
Spectrum/William Mebane
Broad impact
Until a few years ago, the idea of curing genetic conditions such as Angelman syndrome seemed outlandish—even irresponsible. No one wanted to sow false hope for families. There is already a dearth of treatments for conditions such as these. Their roots in the brain are complex, and getting gene therapies into the brain poses its own unique challenges. The blood-brain barrier, which protects the organ from harmful substances, complicates the delivery of any potentially therapeutic compound.
But unlike most causes of autism, syndromes such as Angelman, Rett, and fragile X have a clear therapeutic target—at least in theory. They can all be traced to one dysfunctional gene and either too much or too little of the protein it encodes.
In classic gene therapy, researchers insert a working version of a missing or mutated gene into an individual’s cells. Generally, they load the healthy gene onto a harmless virus and inject it into a person; the virus infects their cells, delivering the new gene with it, and the cells begin to produce the missing protein. In 2017, the U.S. Food and Drug Administration (FDA) approved this type of gene therapy for vision loss and two types of cancer, and it has since given the green light to another two gene therapies.
One of these therapies, onasemnogene abeparvovec (marketed as Zolgensma), treats a neurodegenerative condition called spinal muscular atrophy that leads to the death of motor neurons early in life. Babies with the most serious form of the condition rarely live past their second birthday; others are never able to walk. If children receive a one-time infusion of Zolgensma, currently approved in individuals up to age 2, however, their motor neurons take up a working copy of the gene mutated in the condition, bolstering the cells’ survival and staving off the condition’s consequences. The treatment, approved last year, demonstrated that a gene therapy could effectively reach brain cells, courtesy of an adeno-associated virus called AAV9 that crosses the blood-brain barrier.
Traditional gene therapies for Angelman and other genetic forms of autism are still in the early stages of development. But researchers have already delivered a gene for the protein missing in fragile X syndrome to mouse models of the condition. The treatment eased or reversed abnormal motor activity and anxiety problems in the animals in a 2016 study led by pharmacologist David Hampson of the University of Toronto in Canada. Hampson is collaborating with biotech firms to test the therapy in people with fragile X syndrome, which is the most common inherited form of intellectual disability. “There are strong incentives for moving into trials,” he says.
Other therapies in the pipeline aim to control gene expression, and therefore how much protein a cell makes, rather than correcting a faulty gene’s DNA sequence. In one approach, including GeneTx’s treatment for Angelman, short strings of modified DNA or RNA called antisense oligonucleotides home in on a gene’s RNA readout and change or disable its protein-making instructions. A promising feature of these molecules is that they are like switch hitters—they can turn production of a problematic protein on or off as needed.
GTX-102 works by interfering with the natural genetic brake that silences the paternal copy of UBE3A. In effect, it inhibits the inhibitor, thereby activating the gene.
A success in this space will completely change the way that we think about genetic testing in autism.
- Timothy Yu, Boston Children’s Hospital
Three years before Zolgensma, the FDA approved an antisense oligonucleotide for spinal muscular atrophy called nusinersen and marketed as Spinraza. The drug, injected directly into the cerebrospinal fluid, binds to the RNA for a second motor neuron gene that, like the gene targeted by Zolgensma, encodes the protein missing in the condition. The binding alters the RNA’s genetic instructions to boost production of the protein.
Because the drug compensates for, rather than corrects, the condition’s underlying genetic fault, the more than 10,000 people worldwide who get Spinraza shots must take it every four months. But many have either regained or preserved their ability to stand, hold their head up or even walk. And if given early enough, the drug may protect children from the most severe aspects of the condition, or prevent them from developing it, according to preliminary results of a clinical trial that started in 2015.
Yet another strategy makes use of DNA-binding zinc finger proteins to boost the expression of specific genes. In July, Sangamo Therapeutics in Brisbane, California, announced a $720 million partnership with the drug maker Novartis to develop therapies that dial up the expression of three genes linked to autism and intellectual disability, although Sangamo has declined to name which genes the companies are targeting.
And gene-editing techniques might also be tapped to suppress gene expression or even correct mutations. In one study, researchers attached the gene-editing technology CRISPR/CAS 9 to a nanoparticle to disrupt the gene for mGluR5 receptors for the neurotransmitter glutamate, implicated in fragile X syndrome and other forms of autism. And one potential prenatal therapy for Angelman syndrome harnesses the same gene-editing molecules to disable the RNA that muffles expression of UBE3A. In an unpublished study, injecting viruses carrying a CRISPR complex into the brains of fetal mice led to some UBE3A expression in neurons. “It works incredibly well, and it lasts for a long time,” says Mark Zylka, the neurobiologist at the University of North Carolina at Chapel Hill who led the work.
For all the promise of these strategies, moving from mice to people often delivers disappointment. The flagship example is the failure of a clinical trial for a treatment for fragile X syndrome that targeted mGluR5 receptors. Some 40 laboratories had produced promising results in mice. “It looked like the perfect drug to translate into people,” says pediatric neurologist Elizabeth Berry-Kravis of Rush University Medical Center in Chicago, Illinois. “How could it fail?” And yet it did.
In retrospect, Berry-Kravis says, the trial design was flawed — in part because researchers tested the drug in adults and adolescents even though young children are most likely to benefit. “In developmental disorders,” Berry-Kravis says, “the money is in getting the kids as young as possible.”
Chop-chop
Berent was uniquely qualified—and determined—to bridge the gap from animals to people for Angelman. Working at the Animal Medical Center, a research-oriented hospital in New York City, she was well-versed in animal research and regularly collaborated with scientists and doctors to test medical devices in animals. “If I can do anything, I can take that animal work and translate that to humans,” she says.
Her experience as a mother gave her little faith in what medicine might offer without her involvement. From birth, Quincy did not nurse as readily as her older sister had. At 1 month old, she was aspirating milk and struggling to breathe, so her parents took her to the emergency room. She was discharged after 8 days on a feeding tube. But back at home, Quincy’s suckle remained weak. “It was just liquid going into her mouth, and we were lucky that she swallowed it,” Berent says.
She and her husband, also a veterinarian and researcher, grew increasingly distraught reading weekly emails they had signed up for that described developmental milestones they should have been noticing. Doctors kept dribbling out piecemeal answers. Their pediatrician, for example, suggested Quincy’s lazy eye or too little time spent lying on her stomach might explain her motor and sensory delays. Berent and her husband were sure their daughter had a more serious condition.
Even a neurologist the family saw took a narrow view of Quincy’s problems. He looked only for signs of brain swelling—and found none. Against that doctor’s advice, they pursued genetic testing. Several weeks later, in late November, Berent got a call from a doctor who said he had “catastrophic news.” Quincy had Angelman syndrome, he soon told them in person.
Berent had never heard of it. She typed it into Google and found listed all of the characteristics she had seen in her daughter: a lazy eye, a flattened head, feeding problems, even irrepressible good humor. “She was like the poster child for this,” she says. “I realized at that moment that I would always know more about my child and that disorder than any physician would.”
Within days, Berent called Arthur Beaudet, the geneticist who had led the Angelman mouse study when he was at Baylor College of Medicine in Houston, Texas, to find out what the next step was. “Allyson wanted to talk about a cure from the moment she knew what she was dealing with,” he says, recalling their initial conversation. Beaudet explained to Berent that the therapy was in the hands of Ionis Pharmaceuticals, which had provided him with the molecules to test. But the company had a track record of working with parents—it was about to launch Spinraza—and so Beaudet connected Berent with Frank Bennett, chief scientific officer at Ionis, who had helped develop that drug.
How could she help? Berent asked Bennett. He suggested she spearhead efforts to access and verify data on the typical course of the disease. Those data could serve as a benchmark in future clinical trials. Berent got to work but, as time wore on, realized Ionis was unlikely to follow a mother’s timeline, driven solely by urgency. “If you are 50th in the pipeline, when are they going to get to you?” she says. And there were already delays. According to Beaudet, the company was struggling to produce a mouse with the human UBE3A gene to test its oligonucleotides. (An Ionis spokesperson says its Angelman candidate was a priority at the time.)
Over the next few months, though, Berent learned of other groups exploring gene replacement and other therapies for Angelman. As she delved into the science and circulated at conferences, she began to sense a gap in the efforts to jump from the lab to real-life treatments for children such as Quincy.
At a scientific meeting on Angelman in Chicago in 2015, Paula Evans noticed Berent furiously typing up notes and taking pictures of slides. Evans, a former real-estate agent whose daughter has Angleman, established the Foundation for Angelman Syndrome Therapeutics (FAST) based in Downers Grove, Illinois. The actor Colin Farrell, whose son has Angelman, is its de facto spokesperson. But even against that celebrity backdrop, Berent stood out. “I could tell by watching her that she was going to be a force within the Angelman community,” Evans says. And in Evans, Berent saw a like mind: “She had every intent of doing exactly what I hoped would be done,” Berent says.
Evans invited Berent to serve on the FAST board and, by early 2016, to be the foundation’s chief science officer—an unpaid position. Berent was pregnant with her third daughter, running a full-time veterinary practice and juggling various research projects, but she says there was no way she could refuse. In her off-hours and on vacation days, she reviewed the foundation’s research. She and the FAST team created what they called a “Roadmap to a Cure,” which meant supporting six academic research teams on different therapeutic tacks, including antisense oligonucleotides and traditional gene therapy.
To pay for the effort, FAST upped its fundraising, and Berent too brought her money game. She hired a development firm to find big donors and struck up a Facebook friendship with another Angelman parent, who turned out to be part of the family behind Grand Marnier liqueur. In 2016, the Marnier-Lapostolle Foundation donated $5.8 million to FAST. With funding in place, Berent’s job shifted to project manager, keeping all six teams on track. “It kept us on task in an unbelievable way,” says Scott Dindot, a geneticist at Texas A&M University in College Station. “She deserves all the credit.”
“My middle name is ASAP,” Berent says. “Chop-chop.”

Pipetting progress: Researchers are exploring a host of gene therapies for autism-related conditions in the lab.
Spectrum/William Mebane
Control knob
By the time Berent created her road map, another mother, Monica Coenraads, was already 16 years deep into a comparable attempt to cure Rett syndrome. When Coenraads’ daughter Chelsea, now 24, was diagnosed with Rett at age 2, the cause of the syndrome was unknown. Researchers soon discovered the faulty gene at its core: MECP2.
Mutations in MECP2 lead to low levels of functional MECP2 protein, a master regulator of gene expression. As a result, people with Rett have wide-ranging difficulties, such as intellectual disability, motor and breathing problems, and, often, autism. Because MECP2 is on the X chromosome, the condition affects girls almost exclusively. Boys have only one X chromosome and one copy of MECP2. When that copy is mutated, it can cause such severe traits that they rarely live past early infancy.
Like many other girls and women with Rett, Chelsea is nonverbal and cannot use her hands. She is fed through a tube and has frequent seizures. She also has chronic sleep problems and severe anxiety. Although some women with Rett can walk independently, Chelsea never has. “She’s completely dependent on me for everything,” Coenraads says.
Coenraads’ quest began as soon as Chelsea was diagnosed. In 1999, Coenraads created the Rett Syndrome Research Foundation to channel her efforts. Then, in 2008, she started yet another organization, the Rett Syndrome Research Trust, to focus exclusively on finding a cure. Over the past 10 years, she has raised more than $60 million to support research on a host of gene therapies for Rett, including gene replacement and gene editing. In 2014, the trust established a consortium of gene therapy experts and Rett researchers. “Our goal is to try to act as an incubator or accelerator,” Coenraads says. “We’ve been pretty aggressive in terms of funding a number of different strategies, because we don’t know which one is going to work.”
So far, the effort has yielded two gene-therapy candidates. The first, which would deliver a functional MECP2 gene to cells, was supposed to go to trial in 2019. That was put on hold when the FDA accused AveXis, the company running the trial, of data manipulation in connection with another one of its drugs. The company fired several executives and started fresh. In August, AveXis reported to the Rett community that its preclinical studies were almost complete and that it aims to file an ‘investigational new drug’ application, the precursor to a clinical trial, in the coming months.
Taysha Gene Therapies is shepherding the second Rett drug prospect, slated to enter clinical trials sometime next year. Taysha’s technology would also deliver a working MECP2 gene to cells and includes a molecular device that calibrates how much protein is produced. This control is critical: Too little MECP2 protein leads to Rett, but too much results in MECP2 duplication syndrome, a condition that also causes intellectual disability, seizures, and autism traits. The new therapy acts more like a knob than a sledgehammer, says Claire Aldridge, who leads business development at the University of Texas Southwestern Medical School in Dallas, Taysha’s partner in the project.
Coenraads’ organization also supports research on other genetic approaches. Because women with Rett have a healthy, inactive copy of MECP2, some researchers are trying to reactivate it using CRISPR. The enzyme is designed to modify DNA to turn on expression, a technique the same researchers have used successfully with fragile X. Editing RNA represents another strategy, which biochemist Gail Mandel of Oregon Health and Science University in Portland is exploring. She aims to correct the mutation in the RNA transcript for MECP2, using RNA “guides.” The guides escort an editing enzyme into cells, hijacking the natural editing process. The technique—which so far has worked in cultured cells and in mice—eliminates the risk of overexpressing the MECP2 protein because, unlike DNA, unused RNA degrades quickly.
Researchers at Ionis and Baylor College of Medicine are also developing a therapy for MECP2 duplication syndrome in which antisense oligonucleotides silence the extra copy of MECP2 affected people carry. In 2015, the Baylor team showed that delivering the therapy to a mouse model repaired molecular defects characteristic of the condition and eased lethargy, anxiety, and unusual social behaviors in the mice. The technology can be delivered in controlled amounts and is also reversible, Bennett says. “If we happen to overshoot, we can withdraw the drug and [the level of protein] reverses back. That gives us a lot of hope.”
In addition to looking at dose, researchers are also testing the timing of genetic treatments. In some cases, the optimal time may be in the womb. After all, conditions such as Rett, Angelman, and autism all affect how the brain gets built. “We need to go as early as possible,” Zylka says. “Prenatal intervention is going to be the optimal time to treat.” When researchers explored reactivating UBE3A in a mouse model at different phases of development, they found that they needed to turn the gene on before birth to rescue most traits of Angelman.
But other work suggests treating later in life is hardly futile. In 2007, geneticist Adrian Bird of the University of Edinburgh in Scotland created mice with a genetic switch to turn on or off the expression of MECP2. Turning on gene expression dialed down features of Rett syndrome such as motor and breathing problems—even in adult mice. Another therapy for Angelman—the one that inspired Berent in 2014—also showed success in mature animals, raising hopes for treatments delivered after birth.

Parent pioneer: Allyson Berent helped launch a company to produce a genetic fix for Angelman syndrome, her daughter’s condition.
Spectrum/William Mebane
Uncharted space
Around midnight one Friday in April 2017, Berent got a message from Dindot. It was a picture of mouse neurons glowing fluorescent green, with a note that said something like, “You need to see this.” What the glow indicated is that his team had activated the paternal copy of UBE3A in mice using antisense oligonucleotides, the same type of molecules Ionis and Beaudet had tested.
Over the course of a few meetings, FAST board members debated what to do. In three years, they say, they had seen little progress on Angelman therapies from Ionis or any other drug company that had entered the race. “There was no confidence from us that any pharmaceutical company was going to bring something to the clinic,” Evans says.
So the FAST leadership decided to do it themselves: They licensed the patent for the oligonucleotides from Dindot’s lab at Texas A&M and, in December 2017, launched GeneTx with investments from Angelman families and friends. They were in mostly uncharted space—a room full of Angelman parents planning to go head-to-head against veteran drug makers. Berent became GeneTx’s chief operating officer and Evans the chief executive officer, both drawing a salary for their work for the first time.
The science also moved quickly. Over the next year or so, Dindot demonstrated that the company’s drug candidate activated UBE3A in cultured human neurons and in the neurons of live crab-eating macaques, whose UBE3A gene resembles the human one. Meanwhile, Evans enlisted Jennifer Panagoulias, a drug-industry veteran whose niece has Angelman, to help them cross regulatory hurdles at the FDA and get a clinical trial approved. In August 2019, Ultragenyx, a biopharmaceutical company in Novato, California, paid $20 million for an exclusive option to purchase GeneTx, pending the outcome of that trial, which Ultragenyx is funding. The FDA gave the go-ahead to start the trial in early 2020.
Looking ahead, the team could face legal obstacles along with scientific ones. “There may be a patent fight down the road,” Beaudet says. “It’s kind of interesting to watch it all evolve.”
If I can do anything, I can take that animal work and translate that to humans.
- Allyson Berent
One concern is that restoring UBE3A won’t make a difference for all Angelman children, who can have different underlying mutations. Many with a deleted gene, including Quincy, are often also missing neighboring genes on the same chromosome, resulting in a lack of those proteins as well. Whatever happens, Beaudet credits Berent with pushing the field forward. “She definitely has triggered faster movement,” he says.
Also, antisense oligonucleotides must be given repeatedly. Like Spinraza, GTX-102 is injected into the cerebrospinal fluid every 4 months. If it reaches the clinic, it may one day be overtaken by one-time therapies that Berent is also pursuing. A traditional gene-replacement therapy for Angelman, also funded by FAST, is being tested in animals at the University of Pennsylvania, according to James Wilson, who directs the Gene Therapy Program there. A parallel effort at the University of South Florida is inching forward, and the CRISPR-based therapies, which could also be one-time fixes, are several years from human testing.
Though Angelman families dream of cures, any treatment that enables their children to communicate or gives them a measure of independence would be welcomed. “If they talk at all, that’s a huge thing,” Berry-Kravis says. “Being able to walk over different surfaces, being able to use a spoon and fork. These are things that would be meaningful.”
And the GTX-102 trial has enormous significance for neuroscience, Berry-Kravis says. “It will help us a lot with understanding whether we can reverse disorders later in life, and how much.” It may also bring us closer to the day when there is an array of standard gene-therapy technologies that scientists can retrofit to any condition. Many expect researchers will uncover more autism-linked conditions that, like Rett and Angelman, are driven by a single gene. Gene therapies might also be able to treat more complex forms of autism. A next step might be uncovering forms of autism linked to just two or three genes and then targeting those.
Quincy, now 6 and in kindergarten, has applied to participate in the first phase of the GeneTx trial. Quincy can walk, though her balance is poor and she falls frequently. Though she is nonverbal, she knows some numbers and letters and communicates using a picture-based system on a tablet. Quincy spent two years learning to crawl and six years mastering waving ‘hello.’ Like her mother, difficulty does not deter her. Says Berent, “She has taught us so much about life and grace.”
This article was reprinted with permission from Spectrum, the home of autism research news and analysis.
*Correction, 19 October, 3:15 p.m.: A previous version of this article incorrectly stated that Zolgensma is administered via injection. It is delivered through an infusion.