Treatment:
Acceptance and Commitment Therapy for Chronic Pain
2015 EST Status:
Treatment pending re-evaluation
Very strong: High-quality evidence that treatment improves symptoms and functional outcomes at post-treatment and follow-up; little risk of harm; requires reasonable amount of resources; effective in non-research settings
Strong: Moderate- to high-quality evidence that treatment improves symptoms OR functional outcomes; not a high risk of harm; reasonable use of resources
Weak: Low or very low-quality evidence that treatment produces clinically meaningful effects on symptoms or functional outcomes; Gains from the treatment may not warrant resources involved
Insufficient Evidence: No meta-analytic study could be identified
Insufficient Evidence: Existing meta-analyses are not of sufficient quality
Treatment pending re-evaluation
1998 EST Status:
Strong Research Support
Strong: Support from two well-designed studies conducted by independent investigators.
Modest: Support from one well-designed study or several adequately designed studies.
Controversial: Conflicting results, or claims regarding mechanisms are unsupported.
Strength of Research Support
Empirical Review Status
2015 Criteria
(Tolin et al. Recommendation)
(Tolin et al. Recommendation)
Very Strong
Strong
Weak
Insufficient Evidence
Treatment pending re-evaluation
1998 Criteria
(Chambless et al. EST)
(Chambless et al. EST)
Strong
Modest
Controversial
Find a Therapist specializing in Acceptance and Commitment Therapy for Chronic Pain. List your practice
Brief Summary
- Basic premise: By accepting and learning to live with pain, one can limit the control it exerts over his or her life.
- Essence of therapy: This therapy guides individuals to change their expectations from the elimination of pain to living as well as possible with pain. Through metaphors and experiential exercises, individuals learn the futility of control-oriented strategies and the benefits of acceptance-oriented strategies in response to negative internal experiences such as pain and discomfort. Individuals are encouraged to explore their personal values and set goals consistent with those values in order to improve overall quality of life and functioning.
- Length: approx. 8 sessions
Treatment Resources
Editors: Evan Forman, PhD; Joanna Kaye, BA
Note: The resources provided below are intended to supplement not replace foundational training in mental health treatment and evidence-based practice
Treatment Manuals / Outlines
Treatment Manuals
Books Available for Purchase Through External Sites
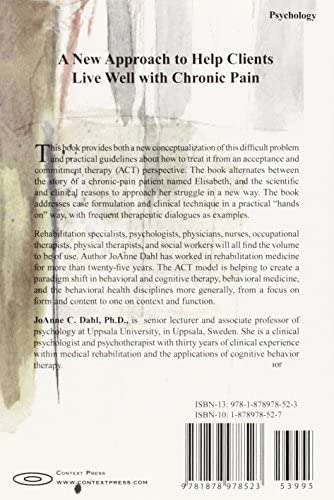
- Acceptance and Commitment Therapy for Chronic Pain (Dahl et al.)
Measures, Handouts and Worksheets
Self-help Books
Important Note: The books listed above are based on empirically-supported in-person treatments. They have not necessarily been evaluated empirically either by themselves or in conjunction with in-person treatment. We list them as a resource for clinicians who assign them as an adjunct to conducting in-person treatment.
Smartphone Apps
Clinical Trials
Meta-analyses and Systematic Reviews
Other Treatment Resources
We are undergoing a revolution in our understanding of human pain and suffering. One of the most promising therapies designed to address human pain is Acceptance and Commitment Therapy (pronounced as “ACT” in one word). Stemming from traditional cognitive behavioral therapy (CBT), ACT is an empirically based, third wave cognitive behavioral therapy that uses acceptance, mindfulness, commitment and behavior change strategies to increase psychological flexibility. The ultimate goal in ACT for chronic pain is to clarify patients’ values so that they can return to a rich, full life.
In many ways, ACT challenges conventional notions of pain management that focus on pain reduction and other “feel good” approaches. ACT for chronic pain is contrary to almost every biomedical approach to alleviating pain— including analgesic medication (opioids, NSAIDS, etc.). These approaches operate under the notion that “pain is bad” and that it must be completely eliminated in order to achieve a free and healthy existence.

A modern exploration of human suffering suggests chronic pain isn’t the enemy and that it doesn’t need to be stopped, fought or controlled. Supported by research in the fields of Relational Frame Theory and Functional Contextualism, the ACT model believes psychological suffering is usually caused by the interaction between human cognition and the control of human behavior through direct experience. ACT protocols target the processes of language that are hypothesized to be involved in suffering and its improvement.
ACT believes that while pain hurts, it is the “struggle” with pain that causes suffering (1).
The ACT approach to living with chronic pain is altogether different and refreshing. It helps patients to accept that while pain may be unpleasant, their lives don’t need to be put on hold in order to manage it. In many ways, ACT works to reverse the negative patterns that many pain patients have endured for years. Attempts to avoid pain can sometimes cause more harm than good, both to the body and peace of mind.
How ACT Can Help Patients Drop the Struggle with Chronic Pain
Acceptance and Commitment Therapy (ACT) emphasizes acceptance and mindfulness paired with commitment action to make lasting changes that will improve quality of life. The three tenets of ACT are:
- Accepting experiences instead of rejecting them simply because they may cause chronic pain.
- Choosing behaviors mindfully versus allowing automatic or conditioned responses.
- Taking action and having agency in your life rather than becoming paralyzed by unpleasant thoughts, memories, emotions or sensations.
ACT and Chronic Pain
Chronic pain often leads to fear, anxiety, and avoidance behaviors, or what is known as experiential avoidance in ACT. Patients stop engaging in activities that they associate with pain, often abandoning hobbies they enjoy. Unfortunately, behaviors like these that are intended to reduce pain can actually wind up causing patients to focus on it even more. By swerving through quick-fix treatments and medications, patients end up spending more time trying to ‘solve’ their pain than they do enjoying life. Pain becomes the center subject and managing it becomes a full-time job. Ultimately, this results in even greater dissatisfaction with life, with equal or more pain.
ACT aims to increase patients’ activity and function, enabling patients to see how they can improve and enjoy their lives without necessarily eliminating their pain. The goal is no longer to reduce pain, but to live a peaceful life in spite of persistent pain. ACT encourages patients to think about what their lives could look like without pain, before helping them to understand that they can live well, with or without it. Committed action is a key part of the treatment and ties into the patient’s personal values. Positive outcomes of ACT include an increase in physical and social activity and a decrease in pain-related medical visits. Acceptance of pain is also linked to decreased anxiety, depression, and disability (2).
Psychological Flexibility— The Heart of ACT

Psychological flexibility encourages patients to stop trying to control their pain and to embrace the face that unpleasant experiences are a part of life. The practitioner does not try to change the patient’s thoughts or feelings about pain. Instead, he or she encourages the patient to approach unpleasant thoughts, emotions, memories, and sensations from a place of acceptance. Psychological flexibility allows a person to be live consciously by committing only to behaviors that have valued ends. In this manner, treatment encourages patients to accept negative feelings such as fear, anxiety, or frustration instead of constantly struggling against them. Psychological flexibility reminds patients to remain grounded in the present without getting hooked by unpleasant thoughts and feelings. Unpleasant internal and external experiences no longer bully behavior or inhibit participation in meaningful activities. Psychological flexibility is targeted through six core ACT processes (3).
The Six Core ACT Processes
- Acceptance
- Cognitive Defusion
- Present Moment Awareness
- Self as Context
- Values
- Committed Action
When using ACT with chronic pain patients, it is important for practitioners to express genuine compassion for their clients by tailoring their exercises to individual needs. Practitioners must openly accept and validate their patients’ feelings and take a compassion-focused and shared perspective. The word acceptance is not used in therapy, rather a skilled therapist helps the patient to clarify their values, then encouraging them to take correct action.
Acceptance
The first part of the ACT therapeutic model lies in acceptance. Before progress can be made, the patient must first demonstrate a willingness to experience some pain while still living the life he or she chooses. Rather than trying to escape pain or its associated unpleasantness, the patient learns to see it as normal (4). Acceptance methods promote the engagement in goal-directed action that may include unwanted feelings and refraining from attempts to control feelings.
Exercise: Build willingness skills
Practitioners help their patients to “build willingness skills.” The goal in this part of the treatment is to show patients that their thoughts and emotions are a natural response to pain. By teaching patients to experience emotions naturally, we help them to understand that enjoyable activities need not be compromised for imagined safety and comfort.

Ask your patients to write down an activity that they want to do but are unable to because of their pain. Ask patients to consider what exactly is holding them back. Have them focus specifically on their emotions and body sensations. Then ask them if there were other times in their life when they felt this way but overcame the emotion for something important. This exercise helps patients understand that they do not have to be controlled by their pain and/or associated feelings. A common example of this is public speaking. (Metaphors can often help patients to better understand acceptance and can be tailored to each individual patient.)
Cognitive Defusion
Thoughts can feel automatic and we don’t even realize their impact on our behavior. Part of diminishing the power of thoughts lies in detaching from them (5). During this step, patients learn to simply notice thoughts as they occur without attaching any significance to them. Thoughts are no longer judged as good, bad, right or wrong. Patients simply acknowledge thought without any judgment. In doing so, they can differentiate between having a thought and getting wrapped up in a thought.
Patients practice skills to become aware of their minds without being obsessed with its preoccupations. To help them do this, you can show them how to see thoughts simply as words without assigned power. In this case, patients are not actually changing or challenging thoughts (traditional CBT) but noticing them and choosing not to allow them to influence or control their behavior. Through this step, they begin to recognize the difference between “thoughts” and “truth or reality.”
Exercise: Adding Labels to Your Thoughts
Sometimes labeling thoughts and feelings can help create emotional distance between you and your thoughts and feelings. For example, instead of thinking “I have unbearable pain today,” you can label this thought by adding the phrase “I am having the thought” in front of it. For example, “I am having the thought that I have unbearable pain today.” What thoughts have you been having lately that are related to your pain?
Focus on an especially difficult thought and really try to believe that it’s true. How does this make you feel? Let’s return to the idea of labeling thoughts. Take the same thought you were just believing and add the phrase “I am having the thought that . . . “ in front of it. How do you feel now? Do you believe the thought more or less? You can add more layers to this, by adding more phrases in front of the thought. For example, “I am realizing that I am having the thought that . . . ” How does this make you feel? Do you still believe the thought or does it feel less a part of you?
Listen to this interview with Dr. Kevin Vowles, PhD onHow To Avoid The Trap Of Negative Thinking Using ACT for Pain
Present Moment Awareness

It can be hard to live in the present moment when suffering from pain. During this step of ACT, the patient tries to remain present, instead of replaying past events or worrying about future possibilities. The patient begins to actively focus on experiences as they are occurring in the moment, in real time, developing an awareness of when his or her focus begins to drift into the past or future and then consciously shifting attention to the present moment.
Exercise: Using Your Senses to Connect with Your Environment
When you are trying to be mindful of the present moment, it can help to use your senses to focus in on your surroundings. Take a deep breath and try to focus on your breathing. Look in front of you and identify three objects in your line of sight. For example, perhaps you see a tree out your window or a framed photograph nearby. Now take another deep breath and relax and pay attention to the sounds in your environment. Can you hear three different sounds if you really focus your attention? Perhaps you can hear birds chirping or the sounds of traffic. Take another deep breath and relax and see if you can feel three different things in or near your body. For example, is the carpet below your feet soft? Or do you notice an itch on your leg? When you perform this exercise, it forces you into the present moment as you pay attention to what lies directly before you.
Listen to this interview with Dr. Lilian Dindo, PhD on How to Use Acceptance And Commitment Therapy To Treat Post-Surgical Pain And Opioid Use In Veterans
Self as Context
In addition to becoming self-aware and remaining aware of the present moment, patients must also learn to notice “self as context” or “the observer self.” Essentially, this means recognizing that their “self” is separate from their thoughts, emotions, or even their physical body. This shift in perspective challenges the self the patient has created—especially when it inhibits positive behavioral change. For example, when a patient allows his or her identity to become entwined with his or her pain. With this practice, patients can learn how to observe their pain without becoming their pain.
Pain mindscripts
Mindfulness is an extremely important, core practice in ACT. It helps establish a sense of self that is greater than one’s thoughts, feelings, body and other private entities. Adopting this point of view also helps with cognitive defusion and enables patients to detach from their own thoughts without being overly influenced by them. Mindfulness exercises can help reduce “pain mindscripts.” For example, I can’t work because of my pain, Any form of exercise will exacerbate my pain, or My pain has to be my priority above all else. When patients learn the “observer self” perspective, as someone who is separate from his or her thoughts, then they can begin to release the mindscripts that are holding them back. Notice your patient’s pain mindscripts so that they can learn to consciously let go of them.
During this part of ACT, patients can learn to release the labels and self-judgments they have created that are not helpful. The following brief exercise can help patients to develop their observer skills.
Exercise: Becoming an Observer Self
In order to better observe your thoughts and feelings and see yourself as a separate entity from them, try the following exercise. Close your eyes and take a deep breath. Become aware of any feelings in your body, whether that’s a pain in your back, an itch on your arm, or simply a feeling of deep relaxation. What thoughts are you having? Simply notice them without judgment. What sounds do you hear going on around you? Recognize that you are paying attention to the feelings in your body, the thoughts in your mind, and the sounds in your environment. Acknowledge that you are separate from each of these things and are simply observing them. Notice the separation from the one who is thinking the thoughts and the one observing the thoughts.
Values
One of the greatest goals of ACT is to help patients pursue their valued activities. This happens when the fear of pain causes a patient to pursue alleviation to an obsessive and limiting extent. Valued activities can include things like exercise, socializing with friends, intimacy with a spouse or partner, going to work, playing with their kids, or being involved in community events. Actions that align with a patient’s values are what bring meaning to that patient’s life.

When patients forsake valued activities for pain control, it often causes them to become depressed. Helping patients identify their values and establish the activities associated with these values enables them to refocus their priorities, away from pain and towards what they enjoy.
To begin this part of the ACT treatment process, ask patients to define their values in major life areas, such as career, family, intimate relationships, friendships, health, and spirituality. Ask them to reflect on what is most important to them.
A potential challenge in identifying values is that patients are likely to perceive how “far” they are from actually embodying them. In this case, the practitioner can show how positive behavior changes can lead patients to better live their values.
Committed Action
Committed Action is the final step of ACT, where patients commit to changing their behavior and taking actions that support their values, in spite of their pain. At this stage, patients begin to develop goals that align with their values. For example, if the “friend” domain is extremely important to one patient, she may choose to engage in more social activities. If the “growth and learning” domain is important to another patient, he may set a goal of taking guitar lessons once a week.
One of the primary issues that arises during this part of the ACT treatment process is dealing with barriers. Perhaps the woman who made a commitment to socializing with friends feels increased anxiety before a lunch date because she fears her back pain will flare up. Or the man who decided to learn a new instrument nearly cancels his guitar lesson because he starts to worry that lessons will conflict with doctor’s appointments and that playing the guitar may worsen his arthritis.
When psychological barriers crop up, it is important for patients to utilize some of the other ACT steps, such as Cognitive Defusion, Present Moment Awareness, and Self as Context in order to remember that they are not their thoughts and feelings. Have patients identify the barriers that do arise in order to help them see what actions they can take to move beyond them.
ACT for Pain Research
Meta-analyses of ACT for chronic pain show improvements in depression, anxiety, pain intensity, physical functioning and quality of life (6,7). Acceptance and commitment therapy for chronic pain is quickly spreading through the mental health and pain psychology fields. There is even some data favoring ACT over traditional CBT!
![]() FREE Download: The 5 Pillars of Pain Care
FREE Download: The 5 Pillars of Pain Care
Dr. Tatta’s simple and effective pain assessment tools.Quickly and easily assess pain so you can develop actionable solutions in less time. Download
Combing ACT with Physical Therapy and Other Disciplines

Combining physical therapy with ACT is one way to create an evidence-based and psychologically informed treatment for patients with pain. A qualitative study investigated potential barriers and facilitators to embedding ACT within a physical therapist-led pain rehabilitation program (8). Findings suggested that this combination presented both challenges and opportunities, but that overall it was a positive experience with sufficient training. Physical therapy treatment, guided by principles of ACT, creates a biopsychosocial treatment for chronic pain that is both evidence-based and innovative (9). Along with CBT and mindfulness, ACT is a psychological intervention that physical therapists and other pain practitioners can use as part of an integrative pain management program (10). The Importance of Embracing Psychosocial Factors of Pain for Physiotherapists will continue to grow.
Studies on physical therapy informed by ACT are just now blossoming and will infuse the physical therapy profession. ACT can seamlessly be integrated into a physical therapy clinical practice and will likely promote better outcomes in pain relief. ACT interventions have also informed the practices of primary care physicians, occupational therapists, nurses, social workers, counselors, corporate health assistants, fitness coaches, health coaches and more (11).
To learn more about ACT for Pain and training for practitioners, click here!
REFERENCES:
Dahl, J., Wilson, K. G., & Nilsson, A. (2004). Acceptance and Commitment Therapy and the treatment of persons at risk for long-term disability resulting from stress and pain symptoms: A preliminary randomized trial. Behavior Therapy, 35, 785-802.
Serbic, D., & Pincus, T. (2017). The relationship between pain, disability, guilt and acceptance in low back pain: a mediation analysis. Journal of Behavioral Medicine, 40(4), 651–658. http://doi.org/10.1007/s10865-017-9826-2
McCracken, L. M., & Vowles, K. E. (2014). Acceptance and commitment therapy and mindfulness for chronic pain: Model, process, and progress. American Psychologist, 69(2), 178-187.
What is acceptance of pain and why would anyone want it?
https://bodyinmind.org/pain-acceptance/
McCracken, L.M., Barker, E. & Chilcot, J. J Behav Med (2014) 37: 1215. https://doi-org.uws.idm.oclc.org/10.1007/s10865-014-9570-9
- M. Veehof, H. R. Trompetter, E. T. Bohlmeijer & K. M. G. Schreurs (2016) Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review, Cognitive Behaviour Therapy, 45:1, 5-31, DOI: 10.1080/16506073.2015.1098724
Öst L-G. The efficacy of Acceptance and Commitment Therapy: an updated systematic review and meta-analysis. Behav Res Ther 2014; 61:105–21. doi:10.1016/j.brat.2014.07.018
Godfrey E, Galea Holmes M, Wileman V, et al. Physiotherapy informed by Acceptance and Commitment Therapy (PACT): protocol for a randomised controlled trial of PACT versus usual physiotherapy care for adults with chronic low back pain BMJ Open 2016;6:e011548. doi: 10.1136/bmjopen-2016-011548
Critchley, D.J. et al. “A light bulb moment!” Physiotherapists’ experiences of delivering Physiotherapy informed by Acceptance and Commitment Therapy (PACT)Physiotherapy , Volume 102 , e230 – e231
Mandy Nielsen, Francis J. Keefe, Kim Bennell, Gwendolen A. Jull; Physical Therapist–Delivered Cognitive-Behavioral Therapy: A Qualitative Study of Physical Therapists’ Perceptions and Experiences, Physical Therapy, Volume 94, Issue 2, 1 February 2014, Pages 197–209, https://doi.org/10.2522/ptj.20130047
Glover, N. G., Sylvers, P. D., Shearer, E. M., Kane, M.-C., Clasen, P. C., Epler, A. J., . . . Jakupcak, M. (2016). The efficacy of Focused Acceptance and Commitment Therapy in VA primary care. Psychological Services, 13(2), 156-161. http://dx.doi.org/10.1037/ser0000062